First Transient Electronic Bandage Speeds Healing by 30 Percent
First Transient Electronic Bandage Speeds Healing by 30 Percent
Bandage also monitors the healing process, alerting clinicians to issues in real time
Feb 22, 2023 - Amanda Morris
Northwestern Engineering researchers have developed a first-of-its-kind small, flexible, stretchable bandage that accelerates healing by delivering electrotherapy directly to the wound site.
In an animal study, the new bandage healed diabetic ulcers 30 percent faster than in mice without the bandage.
The bandage also actively monitors the healing process and then harmlessly dissolves — electrodes and all — into the body after it is no longer needed. The new device could provide a powerful tool for patients with diabetes, whose ulcers can lead to various complications, including amputated limbs or even death.
The research was published online Feb. 22 in the journal Science Advances. It marks the first bioresorbable bandage capable of delivering electrotherapy and the first example of a smart regenerative system.
“When a person develops a wound, the goal is always to close that wound as quickly as possible,” said Northwestern’s Guillermo A. Ameer, who co-led the study. “Otherwise, an open wound is susceptible to infection. And, for people with diabetes, infections are even harder to treat and more dangerous. For these patients, there is a major unmet need for cost-effective solutions that really work for them. Our new bandage is cost-effective, easy to apply, adaptable, comfortable, and efficient at closing wounds to prevent infections and further complications.”

"Our new bandage is cost-effective, easy to apply, adaptable, comfortable, and efficient at closing wounds to prevent infections and further complications." - Guillermo A. Ameer, Daniel Hale Williams Professor of Biomedical Engineering at the McCormick School of Engineering and Surgery at the Feinberg School of Medicine
“Although it’s an electronic device, the active components that interface with the wound bed are entirely resorbable,” said Northwestern’s John A. Rogers, who co-led the study. “As such, the materials disappear naturally after the healing process is complete, thereby avoiding any damage to the tissue that could otherwise be caused by physical extraction.”
An expert in regenerative engineering, Ameer is the Daniel Hale Williams Professor of Biomedical Engineering at the McCormick School of Engineering and professor of surgery at Northwestern University Feinberg School of Medicine. He also directs the Center for Advanced Regenerative Engineering (CARE) and the predoctoral Regenerative Engineering Training Program, funded by the National Institutes of Health. Rogers is the Louis Simpson and Kimberly Querrey Professor of Materials Science and Engineering, Biomedical Engineering, and Neurological Surgery at McCormick and Feinberg. He also directs the Querrey Simpson Institute for Bioelectronics.
Power of electricity
Nearly 30 million people in the US have diabetes, and about 15 to 25 percent of that population develops a diabetic foot ulcer at some point in their lives. Because diabetes can cause nerve damage that leads to numbness, people with diabetes might experience a simple blister or small scratch that goes unnoticed and untreated. As high glucose levels also thicken capillary walls, blood circulation slows, making it more difficult for these wounds to heal. It’s a perfect storm for a small injury to evolve into a dangerous wound.
The researchers were curious to see if electrical stimulation therapy could help close these stubborn wounds. According to Ameer, injuries can disrupt the body’s normal electrical signals. By applying electrical stimulation, it restores the body’s normal signals, attracting new cells to migrate to the wound bed.
"Although it’s an electronic device, the active components that interface with the wound bed are entirely resorbable. As such, the materials disappear naturally after the healing process is complete, thereby avoiding any damage to the tissue that could otherwise be caused by physical extraction." - John A. Rogers, Louis Simpson and Kimberly Querrey Professor of Materials Science and Engineering, Biomedical Engineering, and Neurological Surgery
“Our body relies on electrical signals to function,” Ameer said. “We tried to restore or promote a more normal electrical environment across the wound. We observed that cells rapidly migrated into the wound and regenerated skin tissue in the area. The new skin tissue included new blood vessels, and inflammation was subdued.”
Historically, clinicians have used electrotherapy for healing. But most of that equipment includes wired, bulky apparatuses that can only be used under supervision in a hospital setting. To design a more comfortable product that could be worn around the clock at home, Ameer partnered with Rogers, a bioelectronics pioneer who first introduced the concept of bioresorbable electronic medicine in 2018.
Remote control
The two researchers and their teams ultimately developed a small, flexible bandage that softly wraps around the injury site. One side of the smart regenerative system contains two electrodes: A tiny flower-shaped electrode that sits right on top of the wound bed and a ring-shaped electrode that sits on healthy tissue to surround the entire wound. The other side of the device contains an energy-harvesting coil to power the system and a near-field communication (NFC) system to wirelessly transport data in real time.
The team also included sensors that can assess how well the wound is healing. By measuring the resistance of the electrical current across the wound, physicians can monitor progress. A gradual decrease of current measurement relates directly to the healing process. So, if the current remains high, then physicians know something is wrong.
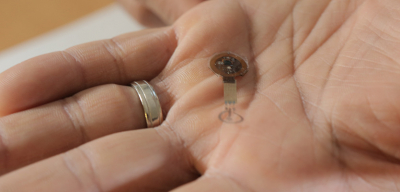
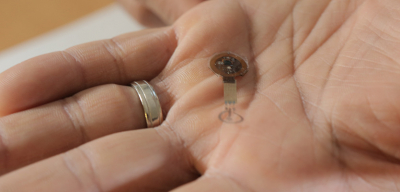
[The device fits easily into the palm of a hand.]
The device fits easily into the palm of a hand.
By building in these capabilities, the device can be operated remotely without wires. From afar, a physician can decide when to apply the electrical stimulation and can monitor the wound’s healing progress.
“As a wound tries to heal, it produces a moist environment,” Ameer said. “Then, as it heals, it should dry up. Moisture alters the current, so we are able to detect that by tracking electrical resistance in the wound. Then, we can collect that information and transmit it wirelessly. With wound care management, we ideally want the wound to close within a month. If it takes longer, that delay can raise concerns.”
In a study of animal models, the researchers applied electrical stimulation for just 30 minutes a day. Even this short amount of time accelerated the closure by 30 percent.
Disappearing act
When the wound is healed, the flower-shaped electrode simply dissolves into the body, bypassing the need to retrieve it. The team made the electrodes from a metal called molybdenum, which is widely used in electronic and semiconductor applications. They discovered that when molybdenum is thin enough, it can biodegrade. Furthermore, it does not interfere with the healing process.
This artistic illustration shows which part of the device dissolves into the body.
“We are the first to show that molybdenum can be used as a biodegradable electrode for wound healing,” Ameer said. “After about six months, most of it was gone. And we found there’s very little accumulation in the organs. Nothing out of the ordinary. But the amount of metal we use to make these electrodes is so minimal, we don’t expect it to cause any major issues.”
Next, the team plans to test their bandage for diabetic ulcers in a larger animal model. Then, they aim to test it on humans. Because the bandage leverages the body’s own healing power without releasing drugs or biologics, it faces fewer regulatory hurdles. This means patients potentially could see it on the market much sooner.
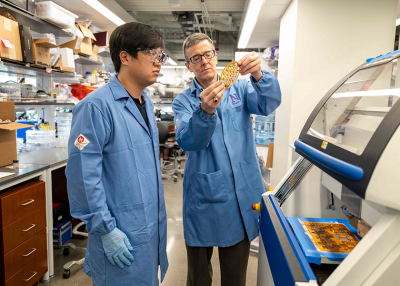
The study, “Bioresorbable, Wireless Battery-Free System for Electrotherapy and Impedance Sensing at Wound Sites,” was partially supported by the National Institute of Diabetes and Digestive and Kidney Diseases and CARE. Northwestern biomedical engineering doctoral candidate Joseph Song is co-first author.
Click here to review the full press release.
A new biodegrading ‘smart’ bandage promises faster healing
The newest smart bandage can stimulate cell growth without overstaying its welcome.
The bandage's molybdenum metal electrodes can safely break down over time. NORTHWESTERN UNIVERSITY
BY ANDREW PAUL | PUBLISHED FEB 22, 2023 4:00 PM EST
We’re used to slapping Band-Aids or gauze on cuts and other gashes, but researchers are exploring higher-tech ideas, too. Micro-thin smart bandages show promise as a potential new method of medical treatment for patients suffering from chronic wounds such as diabetic ulcers. Like some of the tech that has preceded it, the latest iteration leverages electrotherapy to speed up healing time, but goes one step further—it’s capable of safely biodegrading once its task is complete.
Developed by researchers at Northwestern University and detailed in a study published this week with Science Advances, the project’s testing—so far, just in mice—has resulted in the first electrotherapy-delivering bioresorbable bandage, as well as the first example of a smart regenerative system.
Between 15 and 20 percent of diabetes patients will develop an ulcer at some point in their lives. These injuries often go unnoticed due to diabetically induced nerve damage, and are slow to heal due to decreased blood circulation. The longer these wounds remain open or partially healed, the more likely they are to develop serious, sometimes life-threatening complications and infections.
To help cope with this, electrotherapy is a method of stimulating the healing process by attracting new blood flow toward a wound, but the treatment’s required tools and medical instruments have long been bulky, wired (because there needs to be a source for the electricity), and limited to monitored hospital settings. Smart electric bandages could one day soon provide an alternative, saving patients time, money, and lengthy doctor visits.
Here’s how it works: The new, flexible bandage encompasses the site of a wound, and features electrodes on both sides of the material. The inner face includes one electrode that sits atop the injury itself, while its ring-shaped partner surrounds the wound. The other side, meanwhile, hosts a coil to harvest power alongside a near-field communication (NFC) system to wirelessly transmit data. As electric currents ideally help the healing process, additional sensors keep an eye on the progress, and can alert doctors if there are any issues or complications.
During the development stages, the team realized that electrodes made from incredibly thin layers of the metal molybdenum can safely biodegrade over time without impeding the healing process. In their studies on applying the new bandages to mice with diabetic ulcers, the team saw that most of the metal can be absorbed into the rodents within six months, with extremely little accumulation in any of the test animals’ organs. What’s more, healing times increased as much as 30 percent from as little as 30 minutes per day of electrotherapy stimulation.
Once larger animal testing is completed, the team hopes to move onto human trials. Because no drugs or controlled materials are included in the system, it’s possible that the bandage could move into the public sector much sooner than other treatment options needing FDA approval.
Click here to review the full press release.

